Ensuring the safety and sterility of medical devices is essential to protect patient health and meet regulatory standards. Medical device manufacturers are under growing scrutiny to meet strict regulations, especially in aseptic manufacturing, where sterility is a lifesaving requirement.
Maven partners with manufacturers to help them comply with stringent global standards. By offering expert support, Maven ensures companies can manage the evolving regulatory frameworks while maintaining quality, safety, and operational efficiency. This blog explores how aseptic processing regulations have changed, what innovations support compliance, and how manufacturers can adapt proactively.
What is Aseptic Processing?
Aseptic processing refers to the technique of maintaining sterility from the beginning of the production line to the final packaging. It ensures that products, especially those intended for injection or surgical use, are manufactured without introducing contamination at any stage.
Unlike terminal sterilization, which involves sterilizing the product after packaging, aseptic manufacturing keeps all components and environments sterile. This involves:
- Sterilizing raw materials and containers
- Using sterile equipment
- Working in cleanroom environments
- Monitoring environmental conditions constantly
Common products requiring aseptic processing include IV solutions, injectable drugs, and specific medical devices such as catheters. Maintaining sterile integrity during the aseptic manufacturing process is complex and highly regulated.
The Evolution of Aseptic Processing Regulations
Regulations surrounding aseptic processing have evolved dramatically in the past two decades. Initially, the focus was primarily on physical cleanliness, such as filtered air systems, basic microbial testing, and gowning protocols. However, as technology and awareness of risks have advanced, regulatory scrutiny has also intensified.
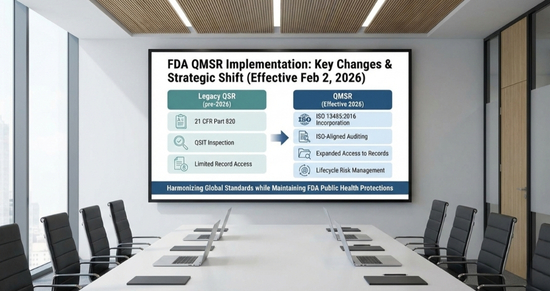
In the U.S., the FDA first released guidance on sterile manufacturing in 1987. The most recent draft of its guidance, titled Sterile Drug Products Produced by Aseptic Processing – Current Good Manufacturing Practice, reflects modern expectations for contamination control, automation, and data integrity. The 1987 guidance has been updated and clarified in this revision.
Globally, regulatory authorities like the European Medicines Agency (EMA) have also updated their guidelines. The revision of Annex 1 in 2022 introduced a more comprehensive approach, requiring manufacturers to adopt a holistic Contamination Control Strategy (CCS) and formalize procedures across the aseptic manufacturing process lifecycle.
Key Regulatory Changes in Aseptic Manufacturing
Let’s see some of the critical updates in aseptic manufacturing regulations that manufacturers must now follow:
- Risk Management Integration: Manufacturers must perform risk assessments at every step, from material sourcing to final packaging, to identify and mitigate contamination risks.
- Contamination Control Strategy (CCS): Regulatory bodies now require a detailed CCS that outlines how sterility will be maintained. It must be tailored to each facility and reviewed regularly.
- Increased Emphasis on Personnel Training: Human error remains a top cause of contamination. Updated guidelines demand better training programs, ongoing assessments, and stricter gowning procedures.
- Environmental Monitoring: Enhanced monitoring of air quality, surface contamination, and microbial presence is now required. Records must be traceable and tamper-proof.
- Validation of Single-Use and Closed Systems: These systems offer strong advantages but require formal validation to prove sterility and compatibility.
Adapting to these changes means conducting risk assessments at every step, developing a comprehensive contamination control strategy, strengthening personnel training, enforcing rigorous environmental monitoring, and validating single‑use and closed systems capabilities that Maven delivers with expertise and reliability.
Digitalization and Automation: A Regulatory Perspective
One of the most prominent shifts in recent years is the emphasis on digitalization and automation. Regulatory bodies now view these technologies as essential to compliance and risk reduction, not merely operational upgrades.
Automated aseptic filling systems, robotic arms in cleanrooms, and real-time digital batch records all contribute to higher process control. The implementation of digital systems significantly reduces human-induced contamination risks in inspected facilities.
Automation also simplifies traceability; each step in the aseptic manufacturing process is recorded, timestamped, and auditable. This aligns with the FDA’s push for data integrity and transparency.
Maven works closely with manufacturers to integrate these technologies while ensuring that validation and regulatory expectations are met.
Advanced Technologies Supporting Regulatory Compliance
As standards become more demanding, companies turn to new technologies to remain compliant without sacrificing efficiency.
Environmental Monitoring and Contamination Control
Real-time monitoring systems now replace traditional microbial tests. These include:
- Automated particle counters
- Real-time microbial sensors
- Predictive data analysis tools
These tools meet and often exceed regulatory requirements, helping teams act proactively. When paired with digital dashboards, monitoring becomes seamless, efficient, and regulation-ready.
Flexible and Modular Manufacturing
The industry is also adopting modular and flexible production environments. These setups allow facilities to quickly adapt to different product types or batch sizes without compromising sterility.
Modular cleanrooms, pre-fabricated isolators, and flexible air handling units support quicker validations and regulatory reviews. These features are essential for smaller or growing manufacturers that need to scale efficiently.
Maven provides end-to-end consultation for implementing modular solutions aligned with industry standards like ISO 14644 and EU GMP Annex 1.
Single-Use Technologies (SUTs) and Closed Systems
Single-use technologies (SUTs) and closed systems are key in contamination control. Because they are disposed of after one use, the risk of cross-contamination is greatly reduced.
Benefits include:
- Elimination of cleaning validation
- Faster product changeover
- Lower operational costs
- Improved operator safety
Regulatory authorities favor SUTs, provided they are properly validated and documented. Maven helps manufacturers with vendor selection, risk assessment, and validation to ensure SUTs are used effectively and compliantly in aseptic manufacturing.
Addressing Challenges in Regulatory Adaptation
While the shift in regulations brings many benefits, it also introduces challenges. Some of the most common include:
- Legacy Equipment: Older systems may not support new validation or monitoring standards.
- Lack of Expertise: Keeping up with regulatory updates across countries requires dedicated knowledge.
- Cost of Upgrades: Investing in automation, SUTs, or digital monitoring involves capital expenditure.
However, failing to adapt to evolving regulatory standards can lead to significant consequences, including regulatory action, loss of market access, or even product recalls. For example, an FDA warning Letter highlights issues such as poor manufacturing practices, misleading product claims, or incorrect usage instructions. The letter allows the company or individual to address the FDA’s concerns and respond within a specified timeframe.
To help organizations navigate these challenges, Maven offers comprehensive support at every stage, starting with gap assessments, followed by training, and culminating in full implementation. This ensures that the adaptation process is manageable and cost-effective, helping companies stay compliant and avoid potential setbacks.
Conclusion
As aseptic processing and sterile manufacturing standards evolve, medical device manufacturers must evolve too. Regulations today are not just rules; they’re a roadmap to better patient safety, stronger process control, and long-term business success.
Digitalization, modular facilities, and single-use technologies are no longer optional but expected. At the same time, staying compliant doesn’t have to be overwhelming.
With Maven’s expert guidance, manufacturers can confidently adapt, improve their aseptic manufacturing process, and stay ahead of regulatory change.
References